Dental Implants: An Integrative Perspective
Michael Baylin, DDSJanuary 30, 2012
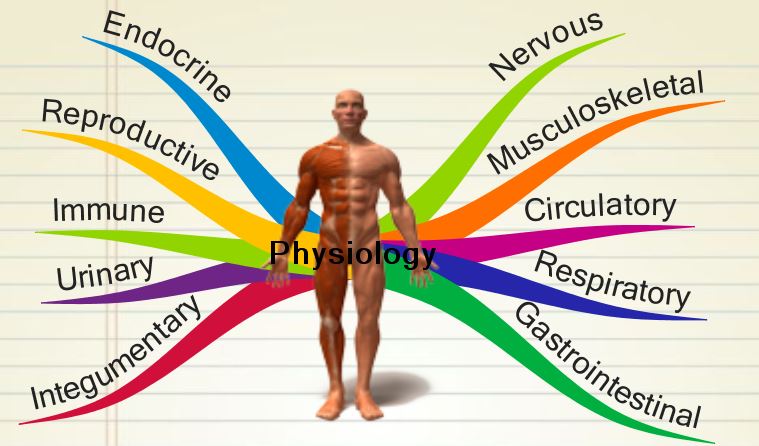
Healthy teeth form the foundation of an attractive face and can be crucial to overall good health. Our teeth influence the functions of eating and speech, as well as affect jaw position and posture. Missing teeth can cause shifting of existing teeth and the collapse of the bite, which can lead to serious health complications including headache, neck pain, and breathing and sleep disorders.
Over the years, dentists have evaluated many practical, comfortable, functional, and affordable ways to replace missing teeth. The option to replace teeth with a removable partial or complete denture is usually straightforward and requires little or no adjustment or grinding of teeth. Commonly, these appliances have a metal framework with clasps to help secure the replacement. Recently, resilient, non-metallic materials have been introduced that are lighter, more comfortable, and aesthetically pleasing.
DENTAL RESTORATION OPTIONS
For a more natural feel, many patients select a fixed bridge to replace missing teeth. The fixed bridge makes good sense when the adjacent teeth needed to support the replacements have large restorations or crowns. Under these circumstances, crowns can actually strengthen weak teeth, and stabilize loose teeth when connecting several teeth together. The most common replacement materials consist of precious or non precious metals with a layer of porcelain fused for function and aesthetics. As with the partial bridges, non-metallic materials are now replacing metals, offering equal precision, strength, and aesthetic appeal.
Dental implants offer another option to consider seriously when replacing missing teeth. Implants have functional and aesthetic advantages. Bridges and removable partial dentures require neighboring teeth as anchors, which can potentially cause damage. However, dental implants can strengthen adjacent teeth and protect and preserve the jaw bone without annoying or unsightly metal clasps. Because implants feel like natural teeth, they offer stability, exceptional chewing comfort, do not constrict the room for the tongue, and are aesthetically natural and healthy in appearance.
Simply stated, an implant is an artificial tooth root, similar to a screw, inserted into the jawbone at the site of the missing tooth. Implants consist of three main parts: the implant itself, the abutment that carries the crown, and the crown, which is the visible portion that looks like the original tooth.
Implants have served patients well for the last forty years, with a retention success rate of approximately ninety-five percent. More than four decades of scientific research and clinical experience have shown that dental implants function as an optimal and permanent solution to tooth loss. Traditionally, titanium has prevailed as the base material for implants because this lightweight and highly resistant metal is well tolerated biologically. Titanium implants, generally placed in two parts, have a range of interchangeable parts and can achieve good aesthetic results, especially on front teeth. The disadvantage of multiple parts is the potential for biofilm accumulation, inflammation, or infection where the different fixtures or parts connect. Additionally, a certain percentage of failures or breakages can occur at the junction of the parts.
ZIRCONIA IMPLANTS
Recently, a new form of dental implants, called ceramic dental implants or zirconia dental implants, offer a potentially more aesthetic and tissue-friendly alternative to traditional titanium implants. Zirconia dental implants are made from special, industrial, high impact resistant ceramic (zirconium oxide, ZrO2) that is customarily used in aerospace engineering because of its high resistance to fracture and heat.
The Food and Drug Administration’s recent approval of zirconia implants opens more options for implants in dentistry. For years, doctors have used zirconia implants to replace hip joints. Ceramic implants retain less plaque and calculus than titanium resulting in healthier gums and overall health. The rough surface of zirconium integrates or attaches itself exceedingly well to the jawbone.
winter2011_baylinfig1Missing teeth, drifting, and bite collapse.
Zirconia implants, fabricated as one piece, can be limiting in their applications. However, the biological, functional, and aesthetic benefits warrant their consideration as a replacement for titanium. Highly stable, biocompatible, and resistant to scratching and corrosion, zirconia is similar in color to natural teeth, creating a more visually pleasing result. It has all the qualities of biocompatibility to make it a material of choice for dental implantation. Additionally, it resists high impact and is non-allergenic.
Zirconium oxide has been used for the past twenty years in hip implants in almost two million patients. Several hundred thousand root posts, crowns, bridges and implant abutments have also been used. In contrast to titanium, zirconium oxide has a significantly higher flexural strength. The flexural strength of zirconium oxide is within 1200-1500 megapascals (units of pressure), approximately three times higher than the flexural strength of titanium at 400 megapascals.
Zirconia implants also offer the crucial advantage of single piece construction. With two-piece titanium implants, the lifetime occurrence of loosening and breakage of the screw connection is 20 percent.
The zirconium oxide used for medical applications is not radioactive and undergoes strict radioactivity monitoring. The maximum level is set at 250 mSv/y (millisieverts per year). The zirconia produced by Metoxit exhibits the lowest radiation levels compared to other manufacturers, and is constantly at 5.4 mSv/y, only marginally more than natural human bone surface at 3.1 mSv/y.
BIOCOMPATIBLE MATERIALS
Biocompatibility is always a key consideration in the dentist’s goal of restoring the patient’s teeth and mouth to optimum health and function. Biocompatibility refers to how a material interacts with the human body and how those interactions determine the clinical success of a medical device. Materials have constantly improved through the years; still, nothing available duplicates the properties of natural teeth or bone. Replacements can be harder, softer, lighter, darker, and biologically compatible or reactive.
Dentists must be concerned with the biological reactivity of the materials they use, as the materials can be toxic or allergic. These responses can be immediate or the effects can accumulate and delay for many years. Reactions to materials vary from patient to patient and can be affected by physiology as well as other materials present in the mouth or even elsewhere in the body. A wide variety of symptoms can occur including local inflammatory pathologies, chronic inflammation including cancers, and various neurologic symptoms, all frequently ascribed to a completely different illness.
winter2011_baylinfig2Metallic removable partial denture.
winter2011_baylinfig3Non-metallic removable partial denture.
winter2011_williamsfig4Two zirconia implants.
winter2011_baylinfig5Two all-porcelain crowns.
REACTIONS TO TITANIUM
If an individual patient’s immune system can compensate for the matrix (connective tissue) contamination by dispersed titanium, then people with titanium implants have no need for concern. However, any indication of possible difficulty requires further investigation including laboratory testing.
Although orthopedists and dentists have implanted many millions of titanium screws without side effects, a small, but significant minority of people experience complications. Cases of intolerance to metal implants have been reported over the years; removing this material resulted in long-term health improvement.
One study investigated fifty-six patients who developed severe health problems after receiving titanium dental implants. The array of medical problems included muscle, joint, and nerve pain; chronic fatigue syndrome; neurological problems; depression; and skin inflammation. Removing the implants resulted in a dramatic improvement in the patients’ syndrome.
In one case, a fifty-four-year-old man with a titanium dental implant and four titanium screws in his vertebra became so sick he could not work. Chronic fatigue syndrome, cognitive impairment, Parkinson’s-like trembling, and severe depression plagued him. Six months after removing the implants and screws, he was well enough to return to work.
A fourteen-year-old girl developed inflammatory lesions on her face six months after receiving titanium orthodontic brackets. Her reactivity to titanium skyrocketed, and she became mentally and physically exhausted. Within nine months after replacing the brackets with metal-free material, her facial lesions almost completely disappeared and she was healthy and active.
Implanted titanium also carries the potential to induce neoplasia (the abnormal proliferation of cells), which could be a precursor to developing malignant tumors. In August 2008, two articles appeared in the Journal of the American Dental Association that discussed two different types of oral cancer. Both articles indicated that dental implants caused or exacerbated the malignant condition.
BATTERY-MOUTH
Titanium implants constantly release metal ions into the mouth. This chronic exposure can trigger hypersensitivity, inflammation and allergies, as well as autoimmune disease in people with high sensitivity. The metal implants can become part of a charged battery. All that is needed to make a battery is two or more different metals and a liquid medium (electrolyte) that can conduct electricity. Metal implants, fillings, crowns, partials, and orthodontic appliances provide the dissimilar metals, and saliva in the mouth serves as the electrolyte. This phenomenon, called “oral galvanism,” creates two major concerns.
First, the electrical currents increase the rate of corrosion (or dissolution) of metal-based dental restorations. Even precious metal alloys continuously release ions into the mouth due to corrosion, a process that gnaws away at the metal’s surface. These ions react with other components of the body, leading to sensitivity, inflammation, and, ultimately, autoimmune disease. Increasing the corrosion rate, therefore, increases the chance of developing immunologic or toxic reactions to the metals.
These electrical potentials, especially those developed by implants, set in a chronic, degenerative and inflamed section of the bone, can disturb local physiology and affect the body’s entire regulatory ability through osseous, lymphatic, immune, vascular, endocrine, autonomic nervous and meridian systems.
A second concern is that some individuals are very susceptible to these internal electrical currents. Dissimilar metals in the mouth can cause unexplained pain, nerve shocks, ulcerations and inflammation. Many people also experience a constant metallic or salty taste, a burning sensation in the mouth, and insomnia.
The higher the current, the faster mercury is being released.
SAFER ZIRCONIA IMPLANTS
Patients need information and coaching to understand whether dental implants are their best solution. They must have comprehensive advice about preconditions and the risks of implant therapy. The dentist assesses the condition of the oral cavity, teeth, and gums in general, and particularly the bone structure. If inadequate bone exists for firmly anchoring the implant, other methods including bone grafting may be required.
Patients can significantly help to ensure the long-term success of the implant. Implants, as with natural teeth, require consistent dental hygiene and healthy and strong bone and gums. Although implants are very durable and capable of lasting for a lifetime, the patient must still maintain the health of the mouth and entire body in order for continued success.
Reasons for failure of dental implants can include poor patient selection—smokers, poor healers, inadequacy of bone, or the improper manipulation of soft tissue and bone. Corrosion of metals over a long time can cause breakdown and loss of the implant as well as health problems for the patient. Additionally, different medications can affect the implant treatment, and a comprehensive medical history is important to ensure implant success.
Because they are highly biocompatible with the human body, high-impact ceramic (zirconium oxide) implants provide a viable alternative to metal (titanium) implants. The ceramic implants have already made their mark for years in Europe and South America. Studies show that the osseointegration—the process of bone growing right up to the implant surface—of zirconia and titanium implants is very similar, and that zirconia implants have a comparable survival rate, making them an excellent alternative to metal implants. One recently published study reports a 93.5-97.6 percent success rate after five years for over eight hundred zirconia implants.
Dr. Christoph Arlom expands the focus on implants when he stated: “The durability of the implant as evaluated in five-year studies stands as the conventional benchmark for successful implant systems. However, should durability be the only criterion for evaluating implant systems? Within community medicine, with large populations screened for risks and the progress of illnesses, other questions can be asked. For example, are patient groups with titanium implants or metal dentures exhibiting a higher incidence of fibromyalgia, multiple sclerosis, amyotrophic lateral sclerosis, Parkinson’s disease, Alzheimer’s disease, or other types of dementia when compared to other patient groups with naturally healthy teeth and metal-free fillings and dentures?”
Given all the potential adverse conditions associated with the titanium dental implant, such as metal sensitivity, inflammation, metal corrosion and physical fatigue, the zirconia implant offers a device that is virtually free of those concerns and is aesthetically comparable to natural teeth.
Many of the teeth that we dentists have painstakingly preserved with root canals, pins, posts, and bonded cores can now be replaced with implants without reservation and with more assurance of a healthy, long-term outcome. Studies indicate a greater chance of long term success with an implant and a crown than a root canal tooth restored with a post core and a crown.
3-D COMPUTER IMAGING
Three-D computer imaging is an import tool for dentists performing implants. Using computerized tomography (CT scan) or cone beam technology (CBT), dentists can visualize the placement of dental implants in three dimensions. This enables the dentist to get an advanced, detailed look at the interior sections of the jawbone, surrounding tissues and nerves. A customized scanning guide for obtaining the image of the jaw enables the fabrication of an accurate, computer-generated surgical guide that makes the best use of available bone, minimizes surgery, and avoids potential problems, such as nerve exposure or sinus perforation. The guide makes placing implants easier and safer.
During my years of dental practice, I have only used implants in essential situations to minimize expense and limit the implantation of metal into the jawbone. As a long time conservative provider of dental implants, I am more confident that I can provide a healthy, biocompatible, longterm, functional, and aesthetic replacement for lost teeth. The advent of computer aided surgery and the availability of non-metallic zirconia implants enhances the potential for successful implant placement. Other, more complex factors deal with strengthening the patient’s immune system, which frequently requires lifestyle changes. This key part of surgical intervention requires cooperation of the patient and input from his or her other healthcare providers.
PATIENTS HAVE FINAL SAY
Patients always have the choice not to replace missing teeth, and, depending on their overall health, may accommodate effectively. Comfort, finances and lack of understanding may figure into their decisions, and every dental treatment is a compromise. However, the newly approved zirconia implants (www.z-systems.biz, www.cerraroot.com) offer more options, which make implant placement a more desirable solution.
SOURCES
- Rabin, Steven I., MD; Calhoun, Jason H., MD, FACS, editor: Immune Response to Implants
- Özkurt Z, Kazazoğlu E., J Oral Implantol. 2011 Jun;37(3):367-76. Epub 2010 Jun 14: “Zirconia dental implants: a literature review”
- Depprich R, Ommerborn M, Zipprich H, Naujoks C, Handschel J, Wiesmann HP, Kübler NR, Meyer U., Head Face Med. 2008 Dec 8;4:29: “Behavior of osteoblastic cells cultured on titanium and structured zirconia surfaces”
- Manicone PF, Rossi Iommetti P, Raffaelli L, Paolantonio M, Rossi G, Berardi D, Perfetti G., Int J Immunopathol Pharmacol. 2007 Jan-Mar;20(1 Suppl 1):9-12: “Biological considerations on the use of zirconia for dental devices”
- Oliva J, Oliva X, Oliva JD, Int J Oral Maxillofac Implants. 2010 Mar-Apr;25(2):336-44: “Five-year success rate of 831 consecutively placed Zirconia dental implants in humans: a comparison of three different rough surfaces”
- Elemam RF, Pretty I, ISRN Dent. 2011;2011:640509. Epub 2011 Jun 15: “Comparison of the success rate of endodontic treatment and implant treatment”
- Valencia Zavala MP, Sánchez Olivas MA, Velázquez Sámano G, Sepúlveda G, Flores I, Velazco A, Vega Robledo GB., Rev Alerg Mex. 2010 Nov-Dec;57(6):202-7: “Allergy to materials used in dental procedures”
- Javed F, Al-Hezaimi K, Almas K, Romanos GE., Clin Implant Dent Relat Res. 2011 Mar 17. doi: 10.1111/j.1708- 8208.2010.00330.x: “Is Titanium Sensitivity Associated with Allergic Reactions in Patients with Dental Implants? A Systematic Review”
- Gökçen-Röhlig B, Saruhanoglu A, Cifter ED, Evlioglu G., Int J Prosthodont. 2010 Nov-Dec;23(6):562-5: “Applicability of zirconia dental prostheses for metal allergy patients”
- Lebedev KA, Poniakina ID., Fiziol Cheloveka. 2011 Jul- Aug;37(4):90-7: “The center of pathological (toxic) action of metals in people organisms and a role of galvanic currents in its induction”
- Chaturvedi TP., Indian J Dent Res. 2009 Jan- Mar;20(1):91-8: “An overview of the corrosion aspect of dental implants (titanium and its alloys)”
- Kucerová H, Dostálová T, Procházková J, Bártová J, Himmlová L, Gen Dent. 2002 Jan-Feb;50(1):62-5: “Influence of galvanic phenomena on the occurrence of algic symptoms in the mouth”
- Hisbergues M, Vendeville S, Vendeville P., J Biomed Mater Res B Appl Biomater. 2009 Feb;88(2):519-29: “Zirconia: Established facts and perspectives for a biomaterial in dental implantology”
This article appeared in Wise Traditions in Food, Farming and the Healing Arts, the quarterly journal of the Weston A. Price Foundation, Winter 2011.